The differential diagnosis for shoulder pain is vast, and importantly includes:
- Rotator cuff injury
- Adhesive capsulitis
- Osteoarthritis of the glenohumeral joint
- Acromioclavicular joint disorders
Rotator Cuff Disorders
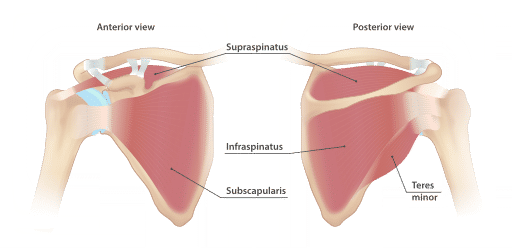
The rotator cuff is a collection of muscles which surround and stabilise the shoulder joint. They are often referred to as the SITS muscles:
- Supraspinatus - 1st 15 degrees of shoulder ABduction
- Infraspinatus - lateral rotation
- Teres minor - ADduction and lateral rotation
- Subscapularis - ADduction and medial rotation
Shoulder impingement/Rotator cuff tendionpathy
- Impingement of the RC tendons beneath the acromion joint causes inflammation/tendinopathy
- Clinical features:
- Aged 35-80
- Subacromial pain - felt at the top and lateral aspect of the shoulder
- Pain is worse when raising the arm
- Night pain might be present
- Triggers: athletes, repetitive movements/lifting (esp. above shoulder height)
- O/E: Painful active/passive ROM, painful arc (70-120 deg), pain on abduction
- Management
- Analgesia
- 1st line: Paracetamol
- 2nd line: Oral NSAID or codeine
- Physiotherapy
- Consider subacromial corticosteroid injection
- Analgesia
Rotator Cuff tears
- Partial or complete RC tears are suggested by severe pain and profound weakness
- Usually occurs in young/middle aged patients following trauma, such as dislocation.
- O/E: Drop arm test may be positive (cannot hold arm up when abducted to 90 degrees)
- Mx: Urgent orthopaedic referral
Adhesive Capsulitis (Frozen Shoulder)
Adhesive capsulitis is a common cause of shoulder pain and stiffness, and is characterised by shoulder pain, followed by progressive stiffness of the shoulder joint. The diagnosis is clinical. Often occurs in the context of diabetes, and thyroid disorders.
Key Features
- Disease/symptom course as below
- Generalised shoulder/deltoid pain and aching
- Gradually progressive stiffness of the shoulder which limits activities of daily living
- Restricted range of movements, especially of external rotation
Clinical course
Adhesive capsulitis is characterised by three phases, each of which overlap to some extent.
- Phase 1 (lasting 3-9 months) - Progressive shoulder pain, especially on movement
- Phase 2 (lasting 6-12 months) - Progressive stiffness and deteriorating range of movement which limits function
- Phase 3 (1-4 years) - Gradual improvement in stiffness and restoration of function
Causes
- Idiopathic (primary)
- Secondary
- DIABETES
- Thyroid disorders
- Trauma + RC disorders
Management
- Analgesia
- 1st line: Paracetamol
- 2nd line: Oral NSAID or codeine
- Refer for PT as soon as possible
- Consider IA steroid injection
Osteoarthritis of the glenohumeral joint
Primary OA of the GHJ is rare as the shoulder is non-weight bearing. Secondary OA is more common, and follows a history of trauma or RC tear.
Key features
- Age > 60
- Deep joint pain
- Globally reduced range of movement, with severe loss of external rotation. This limits ADLs - e.g. putting on a coat.
- Diagnosis: X-ray of the shoulder
Management
- Analgesia
- 1st line: Paracetamol
- 2nd line: Topical NSAID
- 3rd line: PO NSAID or codeine
- Consider IA steroid injection

Acromioclavicular joint disorders
Acromioclavicular joint disorders include injuries of the joint (such as tearing of the ligaments), or osteoarthritis of the joint.
ACJ osteoarthritis
- Age > 60
- Weight lifting is a common risk factor
- Pain is felt over the AC joint
- Pain is worse on lifting the arm up or moving the arm across the body
ACJ injury
- Injury to the joint itself or the surrounding ligaments
- O/E: Localised tenderness of the ACJ and limited range of movement
